WEEKDAYS: 8:00am - 4:00pm. SATURDAY & SUNDAY: CLOSED

Feel Better by Balancing Hormones, Lifestyle, and Mindset
Sick of low energy and other symptoms from thyroid and hormone issues? Tired of hearing "Your labs are normal?"
- Dr. Gibbs specializes in complex hormone problems that have not responded to mainstream medical care.
We are accepting new patients! Virtual or in-Person appointments
Now licensed in IA, MI, KY, GA, TX

Welcome to Consultants in Metabolism, The Medical Practice of Dana Gibbs, MD
Our founder Dr. Dana Gibbs—board-certified ENT surgeon, thyroid expert, and hormone health advocate— combines the best of science, 30 years of medical experience, and whole-person care. Our approach is rooted in data, not dogma. We use advanced testing, T3-inclusive thyroid, menopausal hormone therapies, and targeted lifestyle strategies to restore energy, focus, sleep, and resilience. We believe your symptoms are real, your time is valuable, and your care should be as comprehensive as your story.
“Tired isn’t normal. We help you fix what others missed.”
Unsure about whether thyroid is causing your symptoms?
Get more information about the new Thyroid Clarity Checkup group program - starting soon
Who We Help:


We see patient after patient who are told their labs are fine, and their symptoms must be "in their head", or they are "just signs of getting older". Many others have been mismanaged by providers who claim expertise, but waste money and time on non-covered labs and unproven treatments that don't get you better.
At Consultants in Metabolism, we help patients take back control of their health when standard labs and standard care have failed—through precision testing, expert thyroid and hormone management, and whole-person support.
Who We Help:


Who We Help:
We see patient after patient who are told their labs are fine, and their symptoms must be "in their head", or they are "just signs of getting older". Many others have been mismanaged by providers who claim expertise, but waste money and time on non-covered labs and unproven treatments that don't get you better.
At Consultants in Metabolism, we help patients take back control of their health when standard labs and standard care have failed—through precision testing, expert thyroid and hormone management, and whole-person support.
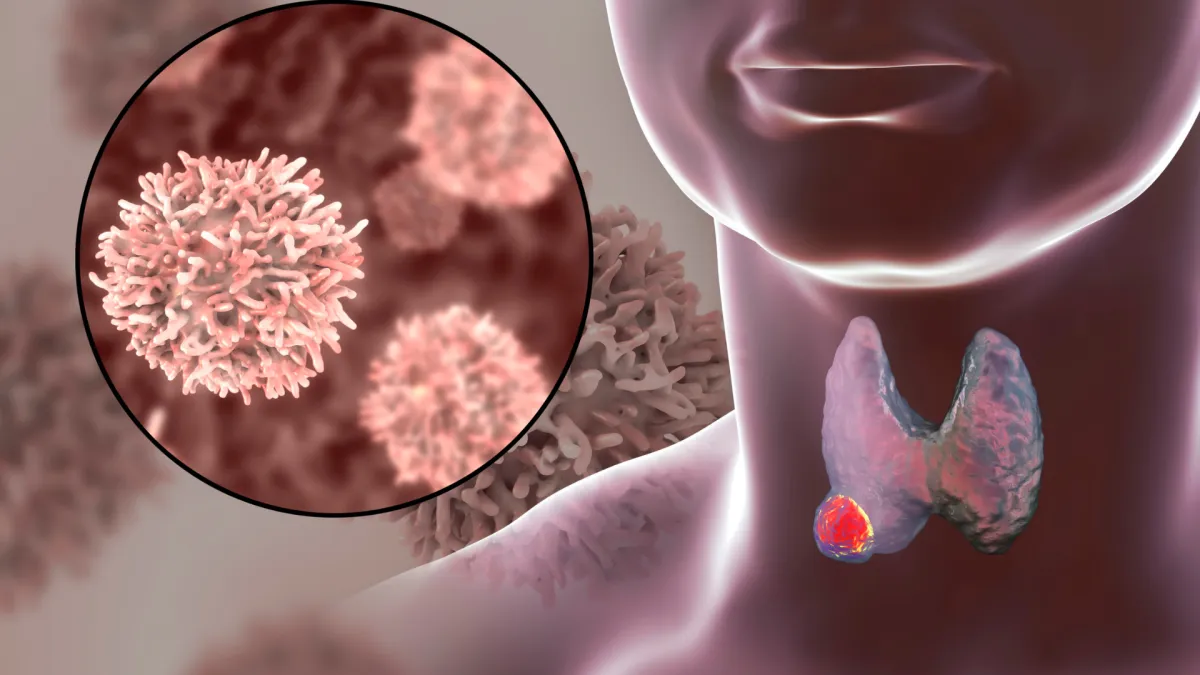
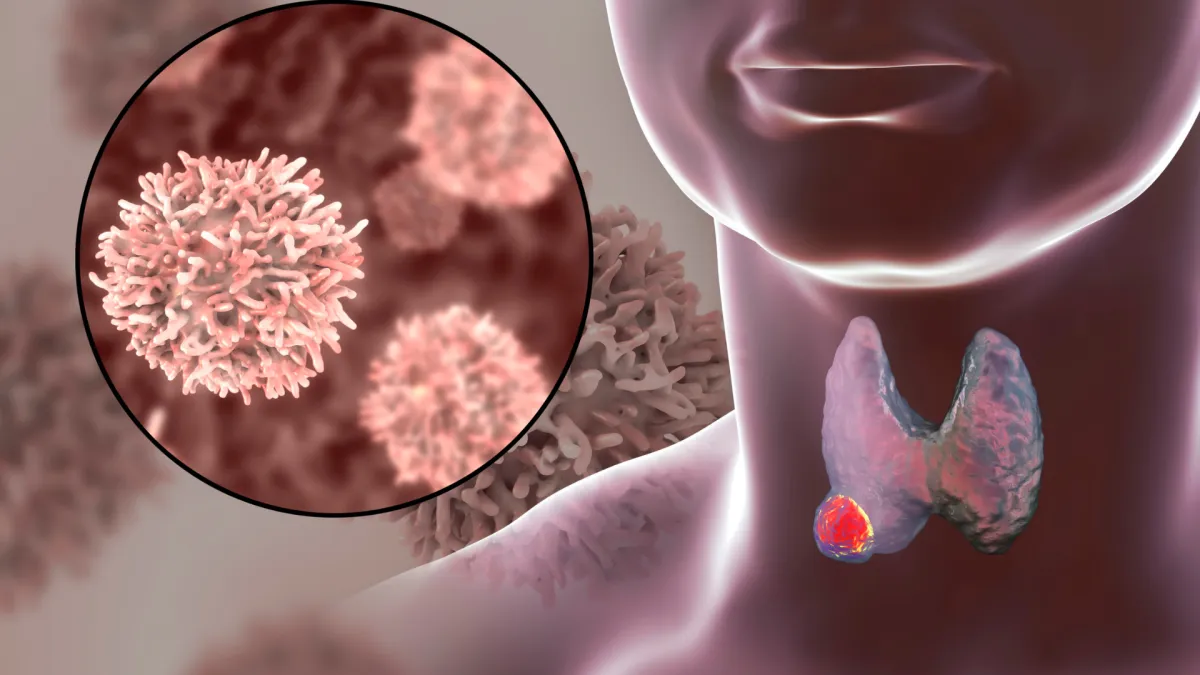
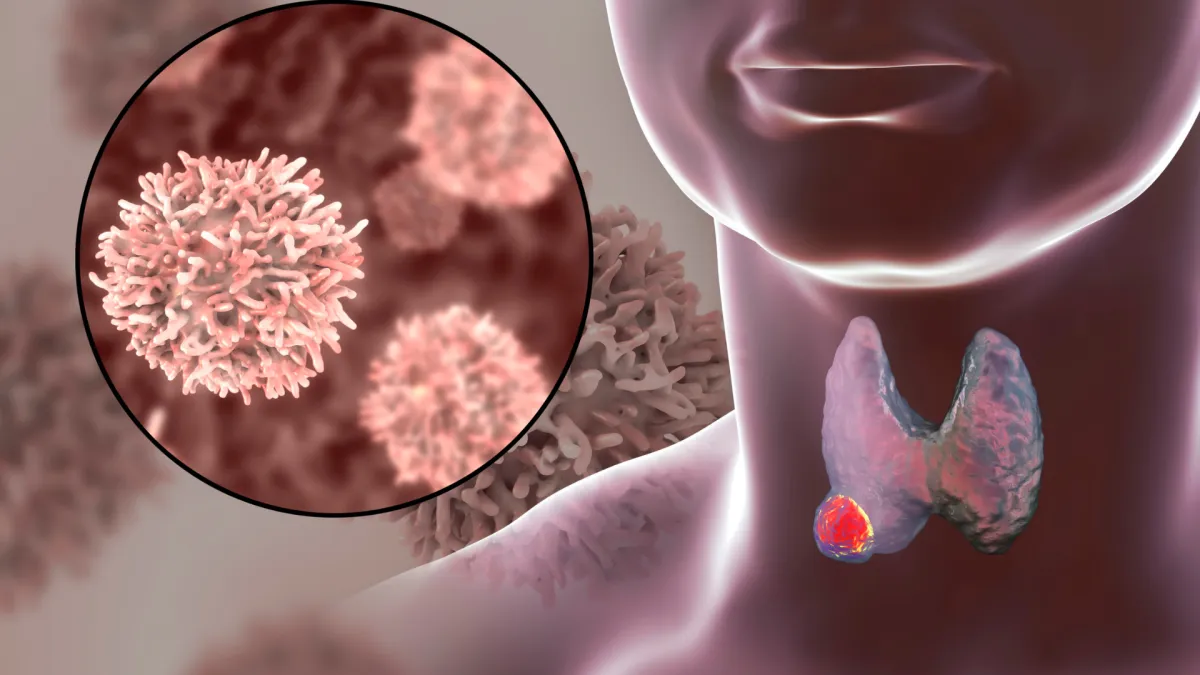
Complex thyroid diseases
Balancing thyroid hormones for optimal energy levels, even in case of "normal" standard labs.
"Brittle" postoperative hypothyroidism
Hashimoto’s disease and Subclinical hypothyroidism
Hyperthyroidism including Graves disease
Hormone Imbalances
Hormone Replacement for Women and Men
Bone health optimization
Perimenopause
Adrenal fatigue - Correcting adrenal overdrive or insufficiency
PMS, PMDD, PCOS
Correct insulin resistance before it becomes diabetes
Chronic fatigue and fibromyalgia
... and More!
What Services Do We Offer?
Services We Offer
Complex thyroid diseases
Balancing thyroid hormones for optimal energy levels, even in case of "normal" standard labs.
"Brittle" postoperative hypothyroidism
Hashimoto’s disease and Subclinical hypothyroidism
Hyperthyroidism including Graves disease
Hormone Imbalances
Hormone Replacement for Women and Men
Bone health optimization
Perimenopause
Correcting adrenal overdrive or insufficiency
PMS, PMDD, PCOS
Correct insulin resistance before it becomes diabetes
Chronic fatigue and fibromyalgia
Adrenal fatigue... and More!
What Services Do We Offer?

Practice Policies

While many services can be provided through virtual visits, sometimes initial encounters need be face to face. The new location in Southlake is accepting new patients! Home visits and alternate locations around the D/FW metro area can be arranged as well.
We are a specialty hormone and thyroid balancing practice. All our patients are required to maintain a relationship with a primary care physician for routine health maintenance and screening...

Practice Policies
While many services can be provided through virtual visits, sometimes initial encounters need be face to face. The new location in Southlake is accepting new patients! Home visits and alternate locations around the D/FW metro area can be arranged as well.
We are a specialty hormone and thyroid balancing practice. All our patients are required to maintain a relationship with a primary care physician for routine health maintenance and screening...

While many services can be provided through virtual visits, sometimes initial encounters need be face to face. The new location in Southlake is accepting new patients! Home visits and alternate locations around the D/FW metro area can be arranged as well.
We are a specialty hormone and thyroid balancing practice. All our patients are required to maintain a relationship with a primary care physician for routine health maintenance and screening...
FAQs
Learn More about CIM Medical
What makes CIM Publishing different from other health services?
xxxCIM Publishing specializes in personalized, scientifically-supported health guidance tailored to individual needs.
How can I schedule an appointment?
The best way to request a new patient evaluation is Online through the MD-HQ Patient Portal link: https://consultantsinmetabolism.md-hq.com .
Click New Patient Registration and create an account. Fill out the New Patient Registration form and add a payment card. Your request will be rapidly approved, and we will contact you to make your initial appointment.
You can also call or message the office at 817-784-7086. Someone will return your call at our earliest opportunity.
What if I'm not sure CIM Medical is right for me?
You can still contact us at 817-784-7086 to arrange an introductory call with Dr Gibbs, or arrange a discovery call by clicking HERE.
We also have a new program called the Thyroid Clarity Checkup, which will walk you through the initial lab ordering and analysis to help you decide if thyroid is part of your problem. Program fee applied to the Accelerate new patient package if you sign up within 90 days of purchase. Click HERE for further information.
Is it possible to cancel or reschedule my appointment?
If you need to cancel or reschedule your appointment, please notify us at least 72 hours in advance by texting or calling {{location.phone}}.
A $100 no-show or late cancellation fee will be assessed if you miss your appointment or cancel less than 72 hours prior. Payment for services is expected in advance of appointments, at the time of scheduling. Failure to provide sufficient notice may result in forfeiture of your appointment fee.
How do I work with you (pricing guide)?
We are out of network for all insurance. Our fee schedule is the same regardless of insurance status.
Medical Visits can currently only be offered to residents of Texas or Iowa. While an initial in-person visit is best, we can also see patients virtually.
If you live out of state, we also offer direct to physician or collaborative consultations if you have a local physician who is interested in working directly with Dr Gibbs.
Dr Gibbs is currently expanding her licensing and collaborating physician network, so don't hesitate to inquire.
Payment for services is expected in advance of appointments, at the time of scheduling. We require a credit card on file to schedule appointments, order labs or other incidental expenses. We accept cash, credit/debit cards, and Health Savings Plan cards. We reserve the right to raise prices at any time.
We have an arrangement for cash-pay labs with Labcorp. It is frequently the case that I can get the recommended labs done for you on a cash price basis at a substantial discount even over your insurance copay, if arranged in advance at the time the order is submitted.
New patient package
ACTIVATE - COMPREHENSIVE NEW PATIENT EVALUATION:
$1200.00 Includes 2 visits:
1. Comprehensive New Patient evaluation, goals assessment, comprehensive history, physical assessment, prior medical treatment review including previous labs, Supplements and Medications review and recommendations, Lab test ordering.
2. Comprehensive follow up visit including plan development, risks and benefits discussion and initial prescribing (prescribing only available in TX and IA.) Follow up planning.
Our per visit NEW PATIENT charges provided outside a membership are based on TIME and COMPLEXITY. We will make every effort to be transparent about these costs. Further a-la-carte services pricing is available on request. Schedule an introductory call for more details.
COMPREHENSIVE FOLLOW UP VISIT $500.00 follow-up for 3 or more treated diagnoses includes interval history review, lab ordering, lab and test review, comprehensive follow-up visit, medication adjustment and plan management. Follow up after initial consultation is recommended at between 4 and 8 weeks.
FOLLOW UP PACKAGES: are available for 6 months at a time.
ACCELERATE - INITIAL SUPPORT PACKAGE: $2300.00
For patients with complex problems. Includes the first 6 months of complete care after the Activate stage is complete, $300 off if purchased at the same time as the initial visit. (Recommended)
Includes step by step plan implementation, medication and supplement adjustments, refinements and additions, as many as necessary to meet the program goals.
Additional follow up appointments involve symptom and goals update, review of ordered tests, interval history, treatment recommendations, informed consent and follow up plan with Q&A.
The ACCELERATE package also includes unlimited access to the physician during business hours to ask questions or report treatment updates via the physician portal or secure SMS messages, phone calls or visits as required.
Access to steeply discounted cash price labs at Labcorp through the physician's GPO.
Access to the physicians' Fullscripts account for discounts on high quality recommended supplements plus seamless ordering.
Includes access to the Master Your Metabolism online education program (check the Courses tab for more details) OR other currently running bonus programs as available such as lessons via video and live virtual: in optimizing hormone levels, supplements, fitness plans, elimination diets, managing blood sugar. These can include documents to track symptoms, labs and med doses over time.
Review and optimize recommended supplements and preferred manufacturers.
This program is also available for stand alone purchase if purchased after your initial appointment date.
MAINTAIN - FOLLOW UP Renewable SEMI-ANNUAL MEMBERSHIP PACKAGE: $750.00 for 6 months or $139/month
Includes ongoing care: questionnaire review, lab ordering, review, as needed follow-up visits, ongoing access though SMS and portal, phone calls, medication adjustments and plan management. This is recommended for at least the first year until all treatment goals have been achieved or if 2 or more visits are anticipated per 6 month time period.
Why can't I use my insurance plan(s)?
We accept patients regardless of their insured status. However we do not participate in any insurance plans. We will be happy to provide medical records and itemized invoices that can be submitted to insurance for claiming of out-of-network benefits. You can submit for reimbursement to your Health Savings Plan or Health Share as well.
.Unfortunately, Dr Gibbs finds it impossible to give the amount of expertise and personal attention you deserve inside the restrictions of an insurance based practice. You will be interacting with Dr Gibbs personally, not a mid-level provider, and your appointment will never be rushed. Furthermore, you will have personal access to the doctor via text and portal message during business hours.
This policy has become necessary due to the increased rate of insurance payment denials after the services have already been provided. In addition, the personal services we offer are not seen to be as valuable as hospital based health care by the insurance companies, which have reduced the offered reimbursement to independent doctors, even in the face of rising costs for staffing personnel, computer systems, supplies, insurance, and rent.
Is there a subscription model for ongoing care?
Yes, we definitely recommend an initial 6 month membership.
ACCELERATE - INITIAL SUPPORT PACKAGE: $2300.00 Includes the first 6 months of complete care after the Activate stage is complete, $300 off if purchased with the initial visit package.
Includes step by step plan implementation, medication and supplement adjustments, refinements and additions, as many as necessary to meet the program goals.
Additional monthly follow up appointments involve symptom and goals update, review of ordered tests, interval history, treatment recommendations, informed consent and follow up plan with Q&A.
The ACCELERATE package also includes access to the physician during business hours to ask questions or report treatment updates via the physician portal or secure SMS messages, phone calls or visits as required.
Access to steeply discounted cash price labs at Labcorp through the physician's GPO.
Access to the physicians' Fullscripts account for discounts on high quality recommended supplements plus seamless ordering.
Includes access to the Master Your Metabolism online education program (check the Courses tab for more details) or Other currently running bonus programs as available such as lessons via video and live virtual - in optimizing hormone levels, supplements, fitness plans, elimination diets, managing blood sugar.
Includes documents to track symptoms, labs and med doses over time. Lists of recommended supplements and preferred manufacturers.
This program is also available for stand alone purchase for a $300 premium if purchased after your initial appointment date.
MAINTAIN - FOLLOW UP SEMI-ANNUAL MEMBERSHIP: $750.00 for 6 months or $139/mo if billed monthly
Includes ongoing care after the first 6 months: questionnaire review, lab ordering, review, as needed follow-up visits.
Unlimited ongoing access during business hours though SMS and portal, phone calls, medication adjustments and plan management.
This is recommended for at least the first year until all treatment goals have been achieved.
Once you are an auto-renewal patient, your rate will never go up, even iwhen pay as you go prices rise.
Testimonials


Laurie Norvik

Dr. Gibbs has been an absolute godsend! After suffering for over 3 years with hair loss, fatigue, brain fog, and poor sleep I have found a physician who actually spends time to diagnose and treat the complex hormonal imbalances that are wreaking havoc on the body. The progress we have made in just 2 months has been life changing. Dr. Gibbs is incredibly empathetic, responds to communication promptly, and is easy to schedule an appointment time with. I can't recommend her enough!


Sara Walker

I was so tired and constantly exhausted, and I had brain fog almost all of the time. I’d done expensive sleep studies and seen other specialists but no one could help me feel better until I started working with Doctor Gibbs. She worked with me and validated me, doing labs and everything she needed to figure out how to treat me, and I feel like a completely new person. No more brain fog or exhaustion!m so grateful for her help—it has been life-changing.


Tessa McCook

I have found the best doctor for my thyroid issues. As many of you know I have Hashimoto’s and it has not been an easy ride. I met Dr Dana Gibbs Clark 11 years ago at Central Park ENT. She has since studied to become a thyroid, hormone and metabolism specialist and has established a new practice called Consultants in Metabolism. She is dedicated to helping her patients get their physical and mental health on track. She’s a stellar physician. I highly recommend her.
Our most popular videos
What is Subclinical Hypothyroidism
Straight Talk About Armour Thyroid
D3 - The Miracle Vitamin
Why Levothyroxine doesn't work for many patients and what to do about it
Click HERE for the complete video library
Our Location
1560 E Southlake Blvd Suite 100, Southlake Tx 76092